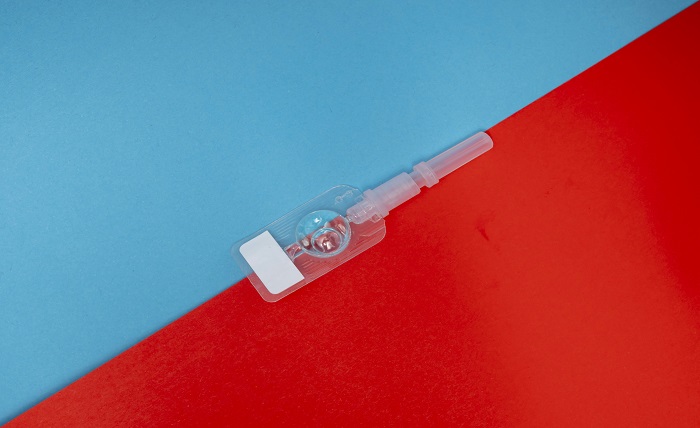
Injectable contraceptives have long been popular choices for women seeking effective and convenient birth control. Each injection is over 99% effective in preventing pregnancy and provides protection for 12 to 14 weeks.
With a single shot, women can enjoy effective contraception without the need for daily pills or frequent medical appointments. However, despite their widespread use, concerns about potential long-term side effects have persisted.
In this article, we aim to explore the existing research on the potential long-term side effects associated with injectable contraceptives.
Weight Gain and Metabolic Changes
A frequently reported side effect of injectable contraceptives is weight gain, which may begin within the first year. The hormonal composition of these contraceptives, particularly those containing progestin, has been linked to alterations in appetite and fat storage. These changes can lead to gradual increases in body weight and shifts in fat distribution, particularly around the abdomen.
According to WebMD, researchers discovered that individuals using the birth control shot for three years gained an average of 11 pounds. In contrast, those taking combined birth control pills during the same study period experienced no weight gain. This highlights a notable difference in weight-related side effects between the two contraceptive methods.
Beyond weight gain, injectable contraceptives may also cause metabolic changes that affect glucose tolerance and insulin sensitivity. Some users have experienced increased cholesterol and markers of metabolic syndrome, raising long-term risks of cardiovascular problems. While not all women are affected, monitoring weight and metabolic health is crucial during prolonged use of injectable contraceptives.
What lifestyle changes can help manage weight while on injectable contraceptives?
Managing weight with injectable contraceptives requires a balanced diet focused on whole foods and minimizing processed sugars. Regular exercise, including cardio and strength training, helps maintain metabolism and muscle mass. Staying hydrated and prioritizing sleep also support overall weight management and metabolic health.
Bone Density Loss
One of the concerning long-term side effects of injectable contraceptives, particularly those containing progestin is bone density loss. These contraceptives can reduce estrogen levels, a hormone crucial for maintaining bone strength. Prolonged use lowers estrogen, which decreases bone mineral density (BMD) and raises the risk of osteoporosis and fractures.
News Medical Life Sciences reported that contraceptive injections reduce bone mineral density by 0.5–3.5% at the hip and spine within one year. After two years of use, the reduction increases to 5.7–7.5%. Following five years, bone density loss stabilizes at 5.2–5.4%.
This effect is particularly concerning for young women during their peak bone-building years and postmenopausal women with weaker bones. Although bone mineral density may recover after stopping the contraceptive, some women could face irreversible bone loss. Extended use without proper monitoring heightens this risk.
Are there preventive measures to take if concerned about bone density loss?
To prevent bone density loss while using injectable contraceptives, ensure you get enough calcium and vitamin D. Regular weight-bearing exercises like walking or strength training, along with avoiding smoking and excessive alcohol, are also essential. Periodic bone density screenings can help monitor bone health and mitigate long-term risks.
Menstrual Cycle Irregularities
Menstrual cycle irregularities are a common side effect of injectable contraceptives. Many women notice changes in bleeding patterns, such as prolonged spotting, lighter or heavier periods, or complete absence of menstruation. These irregularities are often due to the suppression of ovulation and fluctuations in hormone levels caused by the contraceptive.
While some women may welcome lighter or absent periods, others find the unpredictability concerning. These irregularities typically stabilize after a year of continued use but may persist for some users, leading to long-term discomfort or frustration.
Potential Link to Brain Tumors
Emerging research suggests a potential link between the long-term use of injectable contraceptives and an increased risk of brain tumors like meningiomas. These tumors are generally benign but can grow and put pressure on the brain. This may lead to symptoms such as headaches, vision issues, and other neurological problems.
As per TruLaw, a recent study published by the BMJ shed light on new scientific findings. The study revealed that women who received medroxyprogesterone acetate injections, the active component in Depo-Provera, were approximately six times more likely to develop meningioma. This underscores the potential dangers of long-term use of the contraceptive.
Progestin, a hormone in injectable contraceptives like Depo-Provera, is thought to contribute to tumor development. Its impact on hormone-sensitive brain tissues is believed to be a key factor. Although the overall risk remains low, the potential for this serious side effect has led to increased scrutiny.
In fact, concerns over this potential risk have led to legal actions against Pfizer Inc., the manufacturer of Depo-Provera. The Depo Provera lawsuit often alleges that the manufacturers failed to effectively inform consumers about the probable danger of brain tumors. While some of these cases have resulted in settlements, the overall scientific evidence regarding a link between Depo-Provera and brain tumors remains inconclusive.
Increased Risk of Cardiovascular Issues
The overall risk of cardiovascular issues is low in women of reproductive age. However, some studies suggest progestin-only injectable contraceptives may slightly increase cardiovascular event risks.
The risk of cardiovascular issues is affected by several factors, including age, smoking, obesity, and family history. Women with these risk factors should consult their healthcare provider about their contraceptive options. This discussion can help weigh the potential benefits and risks of using injectable contraceptives.
What symptoms should women watch for that may indicate cardiovascular problems?
Women on injectable contraceptives should monitor for persistent chest pain, shortness of breath, dizziness, severe headaches, and swelling in limbs. Unexplained fatigue, rapid heartbeats, or numbness in the extremities may also signal cardiovascular issues. Do not delay seeking medical care if you have any of these signs.
Mental Health Considerations
Injectable contraceptives can influence mental health, particularly mood and emotional well-being. Some women report mood swings, increased anxiety, or depressive symptoms while using these contraceptives, likely due to hormonal fluctuations from progestin. Some women tolerate hormonal changes well, but others may experience negative impacts on mental health, especially with long-term use.
For individuals with a history of mood disorders, side effects may be more pronounced, highlighting the need for mental health monitoring.
Impact on Fertility After Discontinuation
One of the significant concerns for women considering injectable contraceptives is the potential impact on fertility after discontinuation. Injectable contraceptives like Depo-Provera suppress ovulation, which can delay the return of normal menstrual cycles after stopping the injections. This suppression may also impact fertility, making it take longer for women to conceive once they discontinue use.
Many women may experience a prolonged period of amenorrhea or irregular cycles, which can affect their ability to conceive. However, Planned Parenthood reported that pregnancy protection from the Depo shot wears off just 15 weeks after your last injection.
Everyone’s experience is different, and how quickly you can get pregnant after stopping varies. For some people, it may take up to 10 months for fertility to return to normal, while others may conceive much sooner.
Navigating the Long-Term Effects of Injectable Contraceptives
Injectable contraceptives provide a convenient and effective birth control method. While effective, users should be mindful of potential side effects over time. Open conversations with healthcare providers about these risks are essential for informed decision-making.
By understanding both the benefits and drawbacks, women can navigate their reproductive health choices and prioritize their long-term well-being effectively.