Hematopoietic stem cell transplantation is a technique used with increasing frequency for the treatment of many malignant and non-malignant diseases.
Hematopoietic stem cell transplantation involves the collection of bone marrow or peripheral blood cells, either from the patient himself or from a histocompatible donor, and their subsequent intravenous reinfusion, usually after ablative therapy (chemo/radio) to reduce pathological residues. The aim of this technique is to restore blood cell production in patients whose bone marrow or immune system is damaged or defective.
The list of diseases for which stem cell transplantation is used is gradually expanding (currently, over 70 are included), also thanks to advances that have enabled this procedure to be extended to non-malignant clinical situations (as in the case of hemoglobinopathies) and have improved indications depending on the type of transplant (allogeneic, autologous, non-myeloablative).
More than half of autologous transplants (patient-to-patient) are performed for multiple myeloma and non-Hodgkin’s lymphoma, and the vast majority of allogeneic transplants (donor-to-patient) are performed for hematological malignancies and lymphoid malignancies.
Autologous transplantation, stem cell donors and sources
Hematopoietic stem cell transplantation can be performed using cells from the patient (autologous transplant), a sibling, an unrelated donor, or an identical twin (allogeneic or syngeneic transplant). These cells are typically sourced from bone marrow, peripheral blood, umbilical cord blood, or, in rare cases, fetal liver. Each cell source has distinct advantages and disadvantages, with specific clinical applications. Bone marrow transplantation in Turkey, for example, offers a range of advanced options and specialized expertise, making it an attractive destination for those seeking high-quality treatments.
In-depth analysis: what are stem cells and what are their characteristics?
Blood contains a wide variety of cells, each with an essential function to perform:
Red blood cells ( or erythrocytes) transport oxygen throughout the body
Platelets stop bleeding, promoting blood coagulation
White blood cells (leukocytes) are the building blocks of the immune system, protecting the individual from the action of foreign tissues, viruses and various micro-organisms.
All these cells are derived from a single category of founder cells: hematopoietic stem cells, whose main site is the bone marrow.
Hematopoietic stem cells have two fundamental properties:
Self-maintenance: these cells are able to replicate or self-reproduce, keeping their numbers unchanged throughout life;
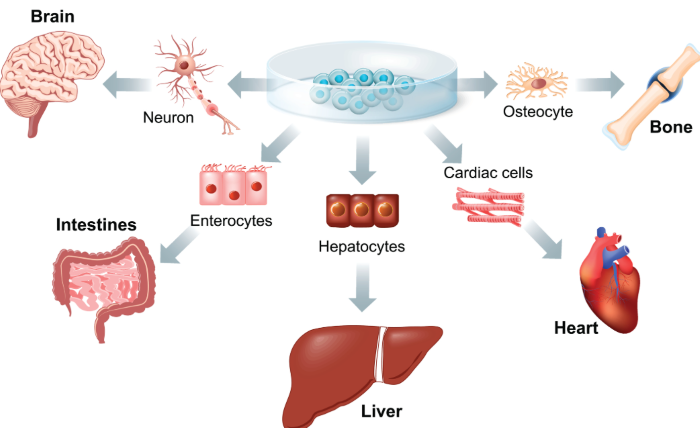
Ability to differentiate.
Thanks to these characteristics, the bone marrow retains throughout the individual’s life the capacity to replace on a daily basis the enormous number of senescent blood cells (after entering the peripheral blood, they undergo a progressive loss of replication capacity). This activity is performed by pluripotent hematopoietic stem cells, morphologically undifferentiated and capable of generating all the mature cells circulating in the peripheral blood. Pluripotent stem cells give rise to daughter cells that follow different pathways:
One will remain in a quiescent state, preventing depletion of the quota of undifferentiated progenitors (equal to around 0.05% of the cells present in the bone marrow);
The latter will undergo a process of differentiation, giving rise to “committed” progenitors oriented in a myeloid or lymphoid direction, progenitors of the various blood supply chains. These progenitors have less evolutionary potential and are not capable of self-maintenance (they are in fact oligo- or uni-potent progenitors).
What is it used for?
Why is a stem cell transplant carried out?
Hematopoietic stem cell transplantation is a procedure designed to replace altered bone marrow with a wealth of healthy cells, obtained from a donor or from the patient himself/herself, capable of reconstituting the recipient’s hematopoietic and immune system.
Hematopoietic stem cell transplantation is often performed as part of treatment to eliminate a bone marrow infiltration process , such as leukemia , or to correct congenital immunodeficiency disorders . In addition, stem cell transplantation is used to enable cancer patients to receive higher doses of chemotherapy than the bone marrow normally tolerates.
Common indications for autologous stem cell transplantation
Autologous stem cell transplantation is used to treat the following conditions:
- Multiple myeloma
- Non-Hodgkin’s lymphoma
- Hodgkin’s lymphoma
- Acute myeloid leukemia
- Neuroblastoma
- Germ cell tumors
- Autoimmune diseases: systemic lupus erythematosus (SLE), systemic sclerosis
- Amyloidosis
- Most common indications for allogeneic stem cell transplantation
Allogeneic stem cell transplantation is used to treat the following disorders:
- Acute lymphoblastic leukemia (ALL)
- Acute myeloid leukemia (AML)
- Chronic myeloid leukemia (CML)
- Chronic lymphocytic leukemia (CLL)
- Myeloproliferative disorders
- Myelodysplastic syndrome
- Multiple myeloma
- Non-Hodgkin’s lymphoma
- Hodgkin’s lymphoma
- Aplastic anemia
- Pure red cell aplasia
- Paroxysmal nocturnal hemoglobinuria
- Fanconi anemia
- Thalassemia major
- Sickle cell anemia